Your role in treating pain an invisible condition
Simply put, self-advocacy is backing yourself. By emphasising your feelings and experiences, you are taking a leadership role in your medical care rather than allowing others to make all the significant decisions. This does not mean being pushy, but it includes asking the right questions so your care provider can address all your health issues.
Of course, self-advocacy begins with building an open and honest relationship with your doctor. Most healthcare professionals enjoy robust dialogue about health issues as it prevents wasted time and effort and focuses treatment.
You may be from a culture that does not like to talk about pain, but you should make every effort to open up about what you are experiencing. Ignoring the issue will not make it disappear, and it could progress into a much worse condition if not adequately addressed. Ultimately, only you can disclose how much pain you are in.
In itself, pain is a medical condition. Your doctor can’t see your pain, although its cause may be apparent in an imaging study, such as a CT or MRI scan. However, you can help your doctor visualise your pain by providing detailed information.
Therefore, asking the right questions is the best way to help yourself in times of chronic pain. So, before you visit your doctor or specialist, preparing a list of questions for the appointment is vital.
Before your doctor’s appointment, think about how you can describe your pain. Make notes and include questions you’d like answered. The suggested questions below can help you analyse and explain your pain.
About Your Pain—Today
- Where is my pain located?
- Does my pain stay in one place or radiate? (e.g., sciatica)
- Does anything specifically trigger my pain? (e.g., sitting, walking)
- Do I experience numbness, tingling, burning, stinging, or electric-like sensations?
- Is my pain constant, or does it come and go?
- How has pain impacted my quality of life? (e.g., hurt relationships, lifestyle changes)
Assessing the Level of Pain
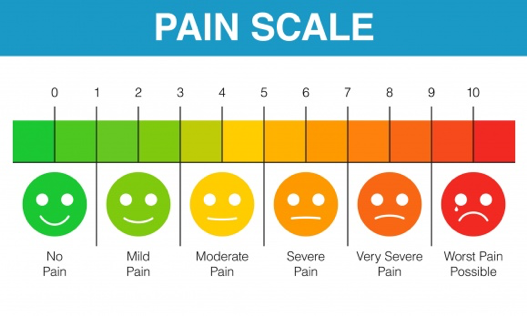
How do I rate my pain on a scale from 1 to 10, with ten being the worst imaginable? (See Pain Scale below)
While the pain scale may provide insight into how intense your pain symptoms are, it does not detail how pain impacts your daily life. Explain to your doctor how the pain interferes with social, professional, and daily activities.
History of Your Pain
- What caused my pain in the first place?
- Did my pain start suddenly or gradually?
- How long have I been in pain?
- What am I currently doing to manage my pain?
- Is there anything I’m doing that’s reducing my pain?
- What pain medications have I taken, and how did they work for me?
- Have I ever had an allergic reaction to pain medication? If so, what were the medicines?
Managing your pain day-to-day
- What are my best hopes for dealing with the pain and treatment?
- What concerns me most about taking medications to help manage pain and other symptoms (e.g., muscle spasms)
- What other activities can I try besides medications that could support my comfort and recovery?
- What other medical conditions do I have? (e.g., diabetes, high blood pressure)
- What are my goals for managing my pain?
Your Appointment
Bring your notes and questions with you to your appointment. Doing so can help you make the most of the time with your doctor and ensure you leave with the information needed to understand your diagnosis and treatment options.
- What’s causing my pain, or is testing necessary to confirm your diagnosis?
- Do I need to see a specialist, or do I need to expand my pain management team to other specialists?
- Can my pain be cured, or should I readjust my expectations to manage my pain?
- What could trigger my pain that I should avoid (such as certain foods or movements)?
- What kinds of pain treatments may be an option for me?
- What are the risks, benefits, and side effects of these treatments?
- What treatment(s) do you recommend I pursue, and why?
- What level of pain relief should I expect from your recommended course of treatment?
- Are there any alternative therapies, such as massage, that I may explore?
- Will lifestyle modifications like diet or exercise help reduce my pain?
More ways to help yourself
Consider bringing a family member or trusted friend with you for support. This kind of support is beneficial if you are the kind of person who does not express pain or discomfort through facial or body language. Your support person can confirm that you are experiencing difficulties due to pain, even if there is no outward expression of distress.
Keep a pain diary.
If you experience ongoing pain, monitoring and recording your daily pain experiences is essential. Write down the intensity of the pain, distinguishing features like burning, itching, tingling or numbness, or any changes in how you are experiencing the pain. Also, note anything that might have triggered your pain, including foods, smells, or bright lights.
If you are reading this and you or someone close to you is suffering from chronic pain, I wish I had something to say that would help/take away the pain, but I don’t. However, I hope these questions help you feel as confident as possible when you meet your healthcare professional.


